
#Nurtec copay card plus#
A recommendation may be presented to the D&T Advisory Board at the earliest opportunity. Prescription copays are different for our Elevate, HDHP, Standard, Elevate Plus and High. Inside Rx cannot be used with any insurance benefit, copay assistance. Reviews are evaluated both clinically and financially. Learn about Nurtec ODT including its uses, possible side effects, interactions.
#Nurtec copay card full#
The review takes place over a three-month period, beginning from the date the drug review is requested. Plus Drug Formulary for the following Department of Managed Health Care (DMHC) plans: Shield Spectrum PPO, Full PPO, Full PPO Savings, Access+ HMO. After BPAS receives the request for a drug review, BPAS pharmacy staff establish the appropriateness of the request. Copay RaAfter your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. To ensure requests for reviews are fair, balanced, and relevant to the Medicaid Preferred Drug List (PDL), BPAS has established procedures for handling these requests. plan uses or have any other questions, call your employers benefit administrator or EmblemHealth Customer Service at the number on your member ID card.
#Nurtec copay card professional#
The Department of Healthcare and Family Services (HFS), Bureau of Professional and Ancillary Services (BPAS) occasionally, receives requests from clinicians in the provider community for individual drug reviews. Eligible patients may pay as little as 0 dollars per month Message and Data rates apply.

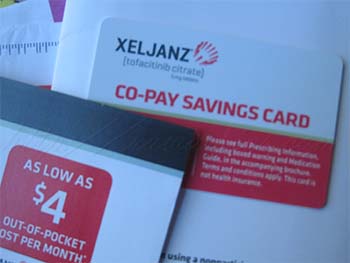
Instructions for Provider PDL Review Requests TEXT NSAVE to 267-89 for a digital Nurtec ODT Savings Card. How do I get the discount Call 1-80 or text NSAVE to 26789 to receive a digital version of your copay card. Subsequent fills: If covered, patient pays 25 for 30 capsules if not covered: patient pays 50 for 30 capsules. First Prescription: Patient pays 0 for maximum of 30 capsules. If it is, you will be contacted by SaveonSP to enroll and lower your. You may register to receive E-mail notification, when a new Preferred Drug List is posted to the Web site, by completing the form for Preferred Drug List E-Mail Notification Request. By using this offer, you are certifying that you meet the eligibility criteria and will comply with the terms and conditions. Accredo determines whether your specialty medication is eligible for co-pay assistance.


 0 kommentar(er)
0 kommentar(er)
